
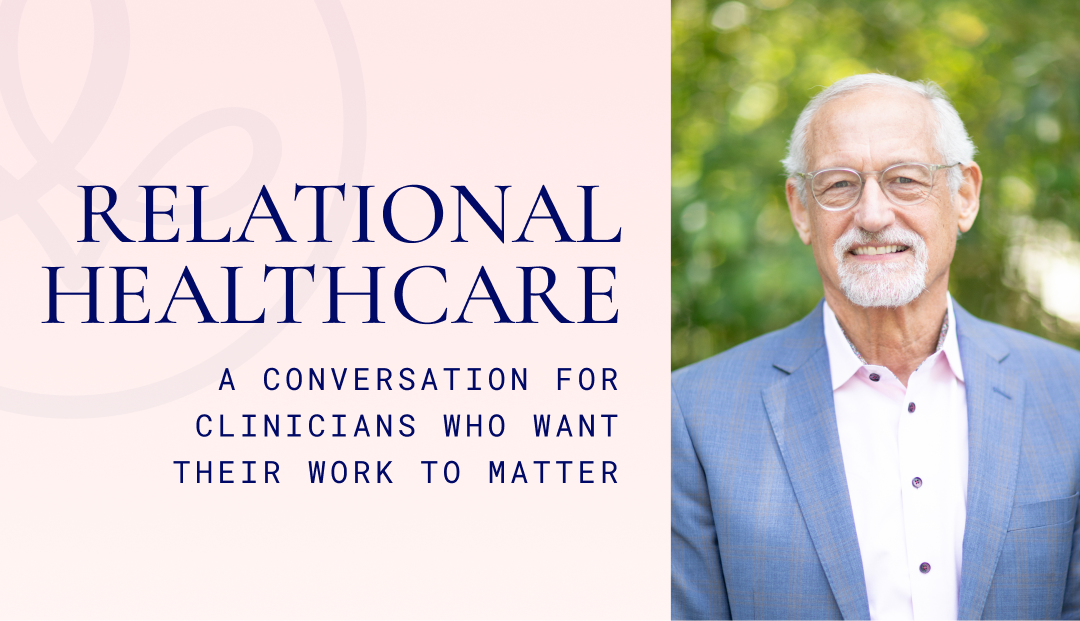
Relational Healthcare: A Conversation for Clinicians Who Want Their Work to Matter
In this conversation, Advaita Health CEO Tripp Johnson sits down with Dr. Dewayne Book, MD, the organization’s Chief Medical Officer, to explore what it truly means to practice relational healthcare. The two have spent years building a model that resists the industry’s drift toward transactional medicine, and this interview offers a candid look at how that philosophy shapes their clinical approach. Dr. Book has been central in defining Advaita’s standards for visit length, continuity, supervision, and team culture. What follows is an honest discussion about the pressures that undermine good care, the commitments required to protect it, and the kind of environment where clinicians can do the work they entered this field hoping to do.
You use the term “relational practice” a lot. People in healthcare throw that around, but you seem to mean something very specific. What is it?
At Advaita Health, “relational” is not an aesthetic or a brand. It’s the center of the work itself. We don’t see patients as units to move through a schedule, or as problems to solve as quickly as possible. We see them as human beings whose healing depends not only on the right diagnosis or the right medication, but on the quality of the relationship they build with their provider.
That’s why our psychiatric evaluations are 60 to 90 minutes. It’s why follow-ups are weekly in the beginning. It’s why we push for continuity, not convenience.
You can’t learn a patient’s history, nervous system, attachment style, trauma imprint, and emotional landscape in a 15-minute med check. You can’t build trust in fragments. And you certainly can’t understand subtle shifts in mood or behavior when the relationship never has a chance to form.
Relational practice requires time, attention, and presence. Those three ingredients are non-negotiable.
You can’t learn a patient’s history, nervous system, attachment style, trauma imprint, and emotional landscape in a 15-minute med check. You can’t build trust in fragments. And you certainly can’t understand subtle shifts in mood or behavior when the relationship never has a chance to form.
And what does that actually look like for patients? What do they feel?
They feel seen. That sounds simple, but anyone who’s worked in this field long enough knows how rare that experience is. Patients come back each week to someone who knows their story, recognizes how they walked into the room today, remembers where they seemed stuck last session, and has the margin to sit with them without rushing.
We pay attention to the quiet signals: when someone suddenly cancels, when they seem guarded or shut down, when they speak differently about themselves than they did three weeks ago. In a transactional model, those things are scheduling issues. In a relational model, they’re data. They’re clues. They’re part of the work.
Patients feel the difference almost immediately. And they stay. Not because we’re “nice,” but because attunement builds safety, and safety is the foundation for clinical change.
Providers often say they want to practice this way, but that the system doesn’t allow it. How does Advaita Health support clinicians internally?
The short answer is: we build the same kind of relationships with our team that we expect them to build with patients. If we reduce clinicians to FTE counts, RVU targets, or interchangeable productivity units, we shouldn’t be surprised when they start treating patients transactionally too. These things are mirrors.
Our medical providers are salaried, not pushed to chase volume.
Our therapists have protected caseloads and clear boundaries.
Supervision is weekly, not twice a year.
And we invest real time in collaboration and consultation.
We’re a deliberately developmental organization because this work is emotionally demanding, intellectually complex, and relationally draining. Clinicians need a place where they can ask honest questions, explore countertransference, reflect on mistakes, and examine how their own nervous system responds inside the clinical room.
A relational culture makes better clinicians. It also makes healthier ones.
We’re a deliberately developmental organization because this work is emotionally demanding, intellectually complex, and relationally draining. Clinicians need a place where they can ask honest questions, explore countertransference, reflect on mistakes, and examine how their own nervous system responds inside the clinical room.
Supervision is a big part of your model, but many clinicians—especially experienced ones—say they don’t need it. Why is it essential?
When someone says, “I don’t need supervision,” what they usually mean is, “I’ve only experienced supervision as policing or oversight.” Real supervision is entirely different.
It’s a protected space to think.
To reflect.
To ask the uncomfortable questions.
To explore why a patient’s anger unsettles you, or why a particular case brings up guilt, or why you feel overwhelmed by someone’s story.
Good supervision makes clinicians more grounded, more confident, and more effective. It also builds safety into the culture: you’re allowed to not know. You’re allowed to name the things that scare you. You’re allowed to be human.
When clinicians feel safe, they do better work. It’s that simple.
You’re explicit that you’re not a private-equity backed group. How does that influence the care?
Everything flows from incentives. If an organization is built to maximize profit, then shorter visits, higher volume, rapid growth, and aggressive leverage are inevitable. Even if no one says it out loud, the culture bends around the financial model.
We built a different structure on purpose.
- Clinicians are paid well, on salary, without volume pressure.
- Visit lengths remain long because they need to be long.
- The organization grows at a pace that protects clinical quality, not investor timelines.
- Decisions are made based on what benefits patients and clinicians—not what hits a quarterly target.
Private equity isn’t inherently evil, but it has a time horizon and a financial mandate that simply doesn’t align with relational care. We’re not building something to sell. We’re building something to sustain.
Clinicians feel that difference immediately.
How would you describe the culture between colleagues, not just patient-provider?
It’s collaborative and honest in a way that surprises people. Providers know one another well enough to ask for help without shame, to consult without defensiveness, to say, “I’m stuck,” or “This case is getting under my skin,” or “I don’t know what this feeling is, but I need to look at it.”
We have regularly protected time where the whole team comes together—not to produce, but to talk, learn, reflect, and simply know one another. Psychological safety isn’t a byproduct here, it’s deliberate. It’s part of the design.
Clinicians shouldn’t feel alone in their work. Not with the stakes of this field. Not with the emotional load they carry daily. We treat team relationships with the same care and seriousness that we treat patient relationships. They’re two halves of the same system.
What makes this model work? Why does it feel so different from high-volume clinics?
Because the incentives, culture, and relationships all align. That’s the piece most organizations miss. You can’t talk about trauma-informed care while pushing providers to see 28 patients a day. You can’t preach “whole-person care” while measuring success exclusively by RVUs.
We designed Advaita Health so that:
- clinicians have time to think,
- patients have time to be known, and
- the organization has time to make decisions that aren’t driven by panic or pressure.
That alignment creates a kind of clinical spaciousness that is extremely rare in modern healthcare.
What kind of clinician thrives at Advaita Health?
Someone who still believes in the work. Someone who gets satisfaction from depth rather than speed. Someone who wants to sit with complexity and knows that the magic is often in the nuance. Someone who values curiosity and humility. Someone who wants to keep growing.
You don’t need to be perfect.
You don’t need to have all the answers.
You do need to care about relationships—both with patients and with colleagues.
If that’s your wiring, you will do the best work of your career here.
You don’t need to be perfect. You don’t need to have all the answers. You do need to care about relationships—both with patients and with colleagues.
And who probably won’t thrive?
Clinicians who want to maximize volume, minimize reflection, and avoid the deeper relational aspects of the work won’t feel at home here. People who prefer transactional, quick-hit clinical care, or who want to practice in isolation, will feel friction. Not because we judge those approaches, but because our structure is built for something entirely different.
If you had to capture the philosophy in one line, what would it be?
We believe healing is relational, and so is good clinical work—and we’ve built a practice that honors both.
Listen to Dr. Book’s Interview with Tripp Johnson:
Closing Note
Ultimately this conversation centers on one question: What happens when you build a healthcare practice around relationships instead of transactions? Dr. Book makes a compelling case that the answer is better care, healthier clinicians, and an organization that actually feels human.