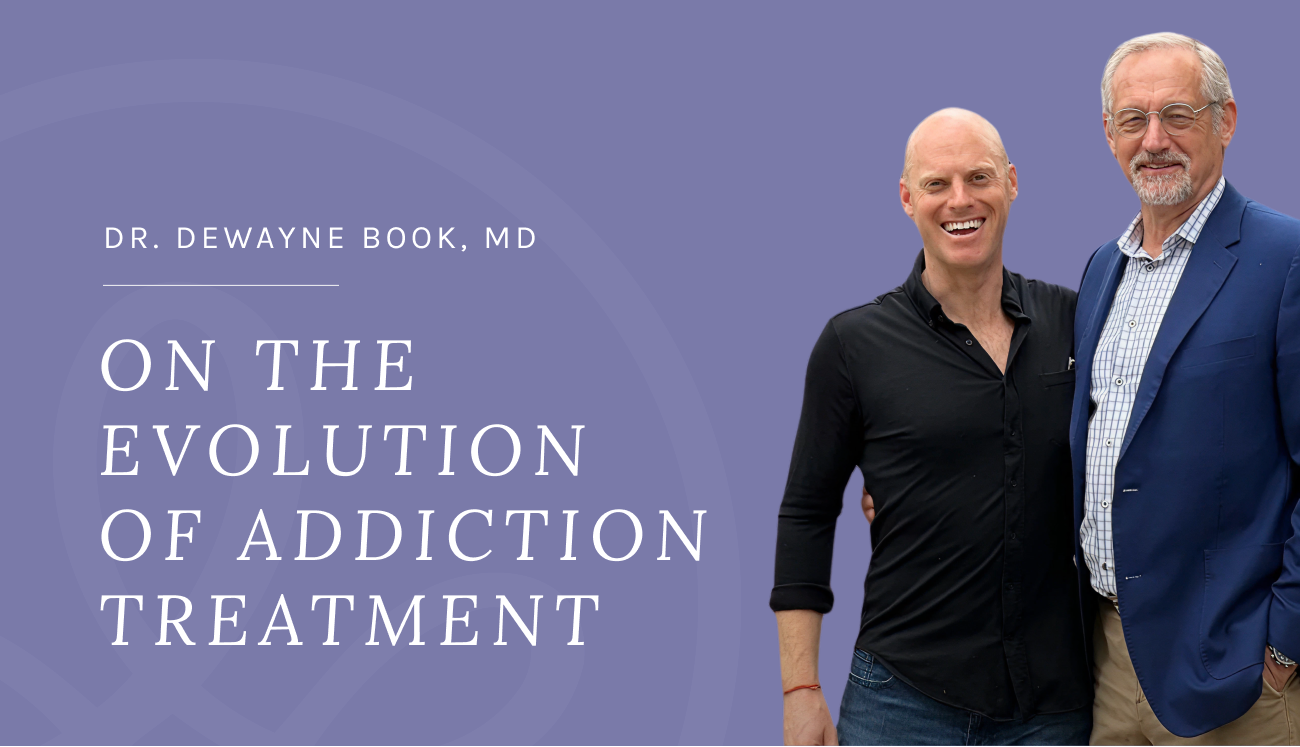
Dr. Dewayne Book, MD on the Evolution of Addiction Treatment
Dr. Dewayne Book’s career in addiction treatment spans nearly four decades, from his start as a newly sober counselor in rural Louisiana to his current role as Chief Medical Officer at Advaita Health. Along the way, he has earned degrees in social work and medicine, helped create Duke University’s first dedicated addiction training track, pioneered the use of buprenorphine in detox at a treatment center, and cared for thousands of patients across residential and outpatient settings. We sat down with Dr. Book to discuss how the field has changed, the role of medication-assisted treatment, and why careful diagnosis in early recovery matters more than ever.
Your first counseling job came with only 10 months of sobriety and a psychology degree. How did that shape your approach?
I didn’t have much formal training back then — what I had was myself. That was enough to show me the central truth of this work: the relationship with the patient is the most powerful tool in the room. Medications and techniques matter, but they only work if the relationship is strong. That philosophy has guided me ever since.
What drove you to keep going back for more education — first a master’s in social work, then medical school?
At every stage, I felt like I didn’t know enough to do what I was being asked to do. As a counselor, I wanted more training and joined a local group of social workers for support. That pushed me toward the MSW. But I also realized that without the MD after my name, I didn’t have access to medications or the same weight in team decisions. Sometimes I knew the patient better than anyone, but the physician had the final say. Going to medical school gave me the tools and the voice I felt patients deserved me to have.
You’ve said the move to Duke nearly ended your sobriety. How did that experience shape you?
Moving is a very high-risk time in recovery. I came close to relapsing on the way to Durham. But I went straight to a meeting and got a sponsor that night. That sponsor later introduced me to Fellowship Hall, where I began moonlighting as a physician. It turned into a three-year job interview, and when I finished residency, I started full-time there. It was a formative experience.
At Duke, you helped establish an addiction training curriculum for psychiatry residents. What was the impact?
When I was a senior resident, our class scored higher on the addiction section of the national in-training exam than any class before us. My classmates said, “It was Dewayne — he taught us what to do.” That gave me the chance to help rewrite the curriculum. We made addiction a required rotation, not just an elective. Every psychiatrist graduating from Duke since 2001 has had a month of focused addiction training at Fellowship Hall. That’s 24 years of residents exposed to this work, and I think that’s one of the most impactful things I’ve been part of.
…The relationship with the patient is the most powerful tool in the room. Medications and techniques matter, but they only work if the relationship is strong.
You also pushed for buprenorphine in detox at a time when it wasn’t widely accepted. What convinced you?
I looked at who was leaving treatment against medical advice. Alcoholics rarely left during detox — because they were given meds to ease withdrawal. Opioid patients left all the time, because we weren’t treating their withdrawal. Once we started using buprenorphine, AMA rates dropped dramatically. Compassion turned out to be good clinical practice.
You often say you use “every tool in the box.” What does that look like in practice today?
I use all the medications available: buprenorphine, naltrexone, disulfiram, acamprosate. Addiction kills 8 out of 10 people who have it. If this were leukemia, no one would withhold chemotherapy. So why would we withhold safe, effective medications for addiction? The relationship is the foundation, but the meds are tools — and I’ll use every one of them to keep a patient alive.
You’ve been in the field since the 1980s. How have the drug epidemics changed over time?
In the ’80s, it was all crack cocaine. I remember being at a clinic for nine months before I saw my first heroin patient — it was that rare. Then came crystal meth in the ’90s, and the devastation it caused was immense. Next was the opioid epidemic, which is still with us. And now we’re dealing with cannabis in a new way: high-potency THC products driving psychosis and anxiety in young people. The drug of choice shifts, but the percentage of people with addiction in the U.S. has stayed stable around 18%. The brain chemistry determines the preference more than the culture.
…Don’t get lost in the computer or the checkboxes. Just be with the patient. If you listen, they’ll tell you everything you need to know. Addiction is often someone’s worst moment — being present for that is the most powerful medicine you have.
You’ve talked about how diagnosing in early recovery can be misleading. Can you share an example?
I had every patient in a 30-day residential program take a Beck Depression Inventory each week. On admission, 99% scored as severely depressed. The other 1%? Either lying or not paying attention — it’s rehab, things aren’t going well. By week four, most patients were no longer depressed at all. That tells you the symptoms were substance-induced. But some groups stood out: those with true comorbid major depression stayed depressed, while others got worse as abstinence unmasked trauma — those were PTSD patients. The lesson is: don’t rush to diagnose everything on day one. Parsimony matters.
So how should clinicians handle early recovery symptoms?
Treat compassionately, but diagnose carefully. Many symptoms resolve with abstinence, and the DSM-5 reminds us: unless better explained by substance use. You can support patients through the suffering without saddling them with half a dozen inaccurate diagnoses. Time and abstinence are part of the diagnostic process.
What advice would you give to young psychiatrists or therapists entering the field today?
Don’t get lost in the computer or the checkboxes. Just be with the patient. If you listen, they’ll tell you everything you need to know. Addiction is often someone’s worst moment — being present for that is the most powerful medicine you have.
Listen to Dr. Book’s Interview with Tripp Johnson:
Closing Note
From counselor to CMO, Dr. Book has spent nearly forty years reminding patients and colleagues alike that addiction treatment is both art and science. Medications save lives, but relationships build recovery.