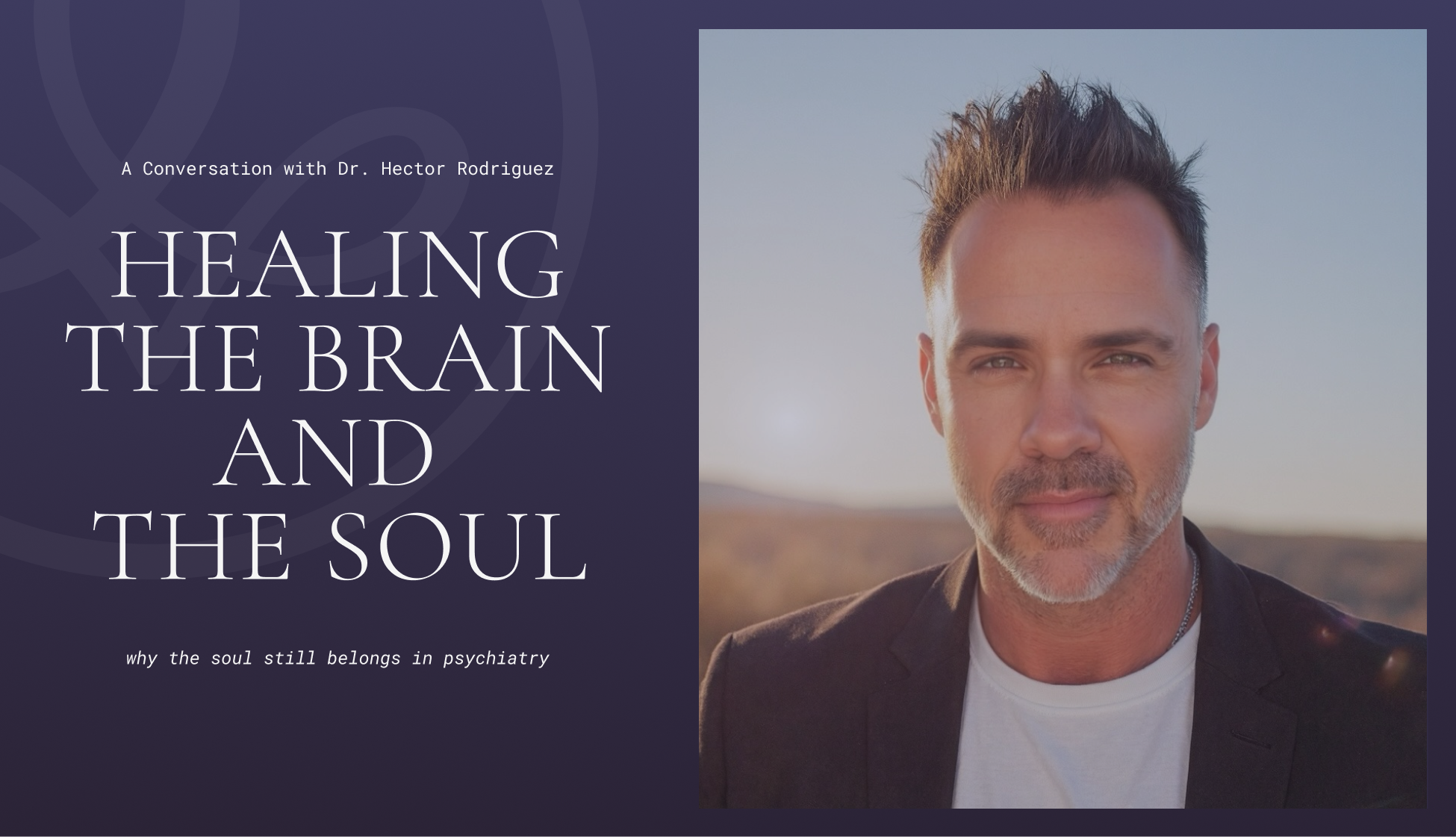
Healing the Brain and the Soul: A Conversation with Dr. Hector Rodriguez
Psychiatrist and executive coach Dr. Hector Rodriguez blends neuroscience, lifestyle medicine, and meaning to help patients move from surviving to flourishing. In this conversation with Tripp Johnson, he shares how trauma shows up in brain imaging, what metabolic psychiatry looks like in practice, and why the soul still belongs in psychiatry.
You have one of the most unusual professional journeys I’ve heard of. How did you go from fashion photography to psychiatry?
I was a fashion photographer for about eight years. I loved the art and creativity of it, but I started noticing something interesting. Before every shoot, I’d spend time getting to know the models, and those conversations would turn into therapy sessions. They’d tell me about their lives, insecurities, relationships—and I realized what I really enjoyed wasn’t taking the pictures, it was connecting with people. That pushed me to go back to medical school and pursue psychiatry.
It was the best decision I ever made. I’ve always been fascinated by human behavior and how people interact. Psychiatry allowed me to combine science with empathy and purpose.
You also have a Master of Divinity. How does that fit into your work?
That came earlier, actually. I’d always been active in my church, and I wanted to deepen my understanding of spirituality and meaning. At the time, I didn’t realize how much it would shape my medical career. Looking back, it’s clear that it helped me see the human experience as more than biology or chemistry—it’s also about purpose, connection, and the stories we tell ourselves.
You trained with Dr. Daniel Amen, who’s known for using SPECT imaging to study the brain. How did that influence your approach?
It completely changed how I see psychiatry. Traditional psychiatry relies heavily on what people report, but self-reporting can be limited. Some patients don’t remember clearly or don’t feel comfortable opening up. When I learned about brain imaging, I saw a way to remove some of that guesswork.
A SPECT scan shows how blood flows through the brain—what’s overactive, underactive, or out of balance. It doesn’t replace conversation, but it adds an objective layer. You can see patterns that correlate with trauma, anxiety, or depression. It’s like having a window into the machinery of the mind.
You’ve said trauma can actually show up in imaging. What does that look like?
When someone has experienced psychological trauma—abuse, neglect, or chronic stress—you often see what’s called the “diamond pattern.” Four regions light up in a diamond shape: the two basal ganglia, the thalamus, and the anterior cingulate gyrus.
The basal ganglia are the anxiety centers. The thalamus regulates circadian rhythms and emotional processing. The anterior cingulate is where people get mentally stuck—looping thoughts, obsessive worry. When those areas over-activate together, you’re looking at a nervous system still on alert.
We also see visual memory patterns when trauma involves witnessing something distressing. The occipital lobe lights up because the brain is still holding the image. What’s incredible is that after therapy, lifestyle changes, and nervous-system regulation, those same scans start to normalize. The pattern softens. The person can literally see their healing.
That’s remarkable. How much of your practice would you say is built around that kind of integrative or functional psychiatry?
It’s central to everything I do. I tell patients that I see all of these approaches as tools in a toolbox. If I only have five tools, I’m limited in how I can help. But if I keep learning—nutrition, movement, peptides, psychotherapy, brain imaging—I can pull out what’s needed in the moment.
I’m still a conventionally trained MD, but I’m always expanding that toolbox. I just came back from a longevity conference in Miami, where we talked about peptides and neuro-optimization. Those things can be powerful, but only once the basics are in place.
What are those basics?
Nutrition first. Remove inflammatory foods like dairy, sugar, and gluten. Focus on a balanced intake of healthy carbohydrates, proteins, and fats—roughly 40/40/20. Then movement, especially high-intensity interval training, which boosts dopamine and executive function.
We check for vitamin and micronutrient deficiencies, especially B vitamins and homocysteine if someone has the MTHFR mutation. We also look for toxins—anything from mold exposure to daily substance use. And sleep follows naturally once the system stabilizes.
You can do all the neurofeedback and hyperbaric oxygen therapy you want, but if you’re drinking heavily or using cannabis every night, your brain stays toxic. The goal is to clean the system first, then optimize.
You mentioned trauma earlier. For people who may not have an obvious “big-T” trauma, how do you help them understand that landscape?
Trauma isn’t just catastrophic events. There are big-T traumas like assaults or accidents, but there are also little-t traumas—the chronic feeling of rejection, being told you’re not enough, losing a job or relationship.
All of that gets recorded in the limbic system. You might not consciously remember it, but the body does. It shows up as anxiety, tension, insomnia, even digestive issues.
What I often see are high-functioning professionals who suddenly start having panic or sleep problems and can’t figure out why. Their body remembers a stressor that feels similar to something from the past. The nervous system goes into fight-or-flight even when there’s no immediate threat.
Trauma isn’t just catastrophic events. There are big-T traumas like assaults or accidents, but there are also little-t traumas—the chronic feeling of rejection, being told you’re not enough, losing a job or relationship.
Lately, trauma seems to be the lens everyone uses. How do you navigate that without over-pathologizing the human experience?
That’s such an important point. The word “trauma” is everywhere now, and in some ways that’s good—it means people are acknowledging pain. But not everything difficult is trauma. Sometimes it’s stress, grief, or just being human.
The key is not to label but to listen. If someone’s suffering, I treat what’s happening. We can explore the origins later. What matters is helping the brain and body feel safe again.
You’re active on social media. How do you think platforms like TikTok are shaping mental health?
It’s a double-edged sword. On one hand, it spreads awareness. People see a post and think, “That sounds like me, maybe I should get help.” That’s great. But there’s also a lot of misinformation. I can’t tell you how many patients come in convinced they have ADHD because of a TikTok clip.
Social media is a popularity contest. The loudest voices aren’t always the most credible. My mentor Dr. Amen told me, “We need more clinicians out there sharing accurate information.” So I try to use it that way—to educate, not sensationalize.
Since you mentioned ADHD, are you seeing changes in attention and focus more broadly?
Absolutely. Our attention spans are shrinking because we’re overstimulated. We’re constantly switching contexts, checking notifications, chasing dopamine. The brain’s filter—the part that decides what to focus on—gets overwhelmed.
I tell patients: take real breaks. Not scrolling breaks. Step outside, close your eyes, pet your dog, breathe. That’s how you reset the nervous system. I practice that myself every day.
You talk about the importance of connection. How do you help patients rebuild that in such a disconnected time?
We are social creatures. The pandemic reminded us of that. When we isolate, cortisol rises and oxytocin drops. I tell people: start hugging again. Physical connection matters.
Recently I went to something called a “coffee party”—no alcohol, just music, yoga, and conversation. It was beautiful. Hardly anyone was on their phone. These moments of community literally heal the brain. Our wiring depends on belonging.
Because of your background in theology, how do you bring spirituality into psychiatry?
The word psychiatry comes from psyche, which means soul. There’s a statue of Cupid kissing Psyche—that’s why my practice is called The White Butterfly. Psychiatry, to me, is the medical treatment of the soul.
You can’t separate the spiritual dimension from the human one. I ask patients to define who they are, what they value, what gives life meaning. Sometimes that leads to prayer, sometimes to reflection, sometimes just to stillness. I don’t impose belief; I invite depth.
We’re not just brains firing neurons. We’re souls trying to make sense of our lives.
You can’t separate the spiritual dimension from the human one. I ask patients to define who they are, what they value, what gives life meaning. Sometimes that leads to prayer, sometimes to reflection, sometimes just to stillness. I don’t impose belief; I invite depth.
What advice would you give to new psychiatrists or clinicians entering the field?
Learn the science, get the credentials, but don’t lose your humanity. Bring your life experience into the room. Show patients that you care and that you’re human, too.
When people feel truly seen, they share things they’ve never told anyone. That’s where the real healing starts. If you’re afraid to sit in the mess with your patients, you’ll never reach them. This work isn’t about perfection—it’s about presence.
Beautifully said. Where can people learn more about your work?
My websites are drhector.com and whitebutterflyclinic.com. We also publish a free online magazine called The White Butterfly Journal and a short workbook series called Power Up. They’re all about building qualities like confidence, discipline, and connection—the foundations of mental wellness.
And of course, I’m on Instagram at @doctor_hector.
Learn more about Dr. Hector’s work:
drhector.com
whitebutterflyclinic.com
@doctor_hector.
Listen to Dr. Hector’s Interview with Tripp Johnson:
